Breast cancer is the most common cancer in women. In the last decades, the life expectancy of breast cancer patients increased substantially due to screening-related earlier detection and advances in treatment. The 5-year net survival is already above 85% in many countries. Radiotherapy is part of the standard treatment as it reduces the risk of recurrences and improves overall survival. However, radiotherapy may lead to serious side effects. Regarding late side effects, retrospective long-term follow-up data of randomised trials have unfold that in particular heart disease and lung cancer are increased after breast cancer radiotherapy. This may be understood as both organs, the heart and the lung, were exposed to high doses during breast cancer radiotherapy in the past. Advances in radiotherapy allow to better spare adjacent organs with modern radiotherapy techniques but doses to the heart and the lung remain to be a major concern. Therefore, two different modern techniques were investigated with regards to the risk induction of ischaemic heart disease and secondary lung cancer, and compared to the standard contemporary technique, the 3D-conformal radiotherapy (3D-CRT).
One of the investigated techniques is the volumetric-modulated arc radiotherapy (VMAT). It allows to conform the therapeutic dose very well to the target volume, and is very valuable to irradiate complex target volumes. The high conformity of the high dose region is achieved by the application of fields from many different directions. However, this has the drawback of an increase of the exposure more remote to the treated breast. The second technique, deep inspiration breath-hold (DIBH) is a specific supplementary technique for breast cancer radiotherapy. During deep inspiration breath-hold the distance between the heart and the irradiated breast increases – which results in a significant reduction of cardiac dose exposure because irradiation is stopped immediately when the patient breathes.
For each of ten left-sided breast cancer patients of the University Hospital of Munich (LMU), four different radiotherapy plans were generated: 3D-conformal and VMAT plans, each for free breathing and DIBH. From each plan, the radiation dose distributions in heart and lung were determined. Epidemiological risk models were applied to estimate resulting risks of heart disease and lung cancer. These models are based on studies of radiotherapy patients after breast cancer and Hodgkin lymphoma, and on low-dose studies. Because there are biologically plausible reasons to assume that lung cancer risk may not be linear with dose, we applied models with a plateau or a downturn of risk at high doses in addition to the linear risk model.
Mean results of the estimated excess risk within 10 years after radiotherapy are plotted in the figure, evaluated for a 50 year old patient. The heart symbols refer to the risk of ischaemic heart disease and are evaluated first for a patient with high cardiovascular risk factors and second for a patient with medium risk. Grey lung symbols refer to the risk of lung cancer, evaluated with the linear model, first for a patient who smokes 30 cigarettes a day and second for a patient who smoked 10 cigarettes a day but quitted recently. Green and blue lung symbols refer to the risk of lung cancer but evaluated with non-linear models.
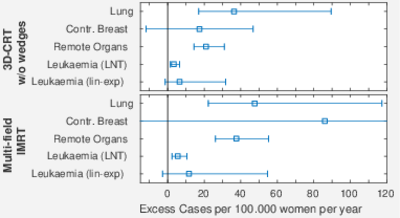
Fig.1: Estimated excess absolute risks within 10 years after breast cancer radiotherapy for different radiotherapy treatment modalities, evaluated for a 50 year old patient. Heart symbols refer to ischaemic heart disease, lung symbols to lung cancer. Different lung symbol colours denote different risk models. EAR: (radiation-induced) excess absolute risk, 3D-CRT: three-dimensional conformal radiotherapy, VMAT: volumetric-modulated arc radiotherapy, DIBH: deep inspiration breath-hold, FB: free breathing.
As can be seen from the figure, the DIBH maneuver resulted in a significant reduction of the estimated 10-year excess absolute risk for heart disease compared to free breathing in 3D-CRT plans. In VMAT plans, the mean risk reduction through DIBH was less pronounced. The risk of radiation-induced secondary lung cancer was mainly influenced by the radiotherapy technique, with no beneficial effect through DIBH. VMAT plans correlated with an increase in risk for radiation-induced lung cancer as compared to 3D-CRT plans. It is important to note, however, that excess absolute risks were affected more strongly by non-radiation-associated risk factors, such as smoking, as compared to the choice of treatment technique.
In conclusion, our results indicate that 3D-CRT plans in DIBH pose the lowest risk for both heart disease and secondary lung cancer but control of standard risk factors is key in reducing late side effects.
Contact: Dr. Cristoforo Simonetto
Publication:
Corradini, S.; Ballhausen, H.; Weingandt, H.; Freislederer, P.; Schönecker, S.; Niyazi, M.; Simonetto, C.; Eidemüller, M.; Ganswindt, U.; Belka, C. Left-sided breast cancer and risks of secondary lung cancer and ischemic heart disease. Strahlenther. Onkol. 194, 196-205 (2018). DOI: 10.1007/s00066-017-1213-y.